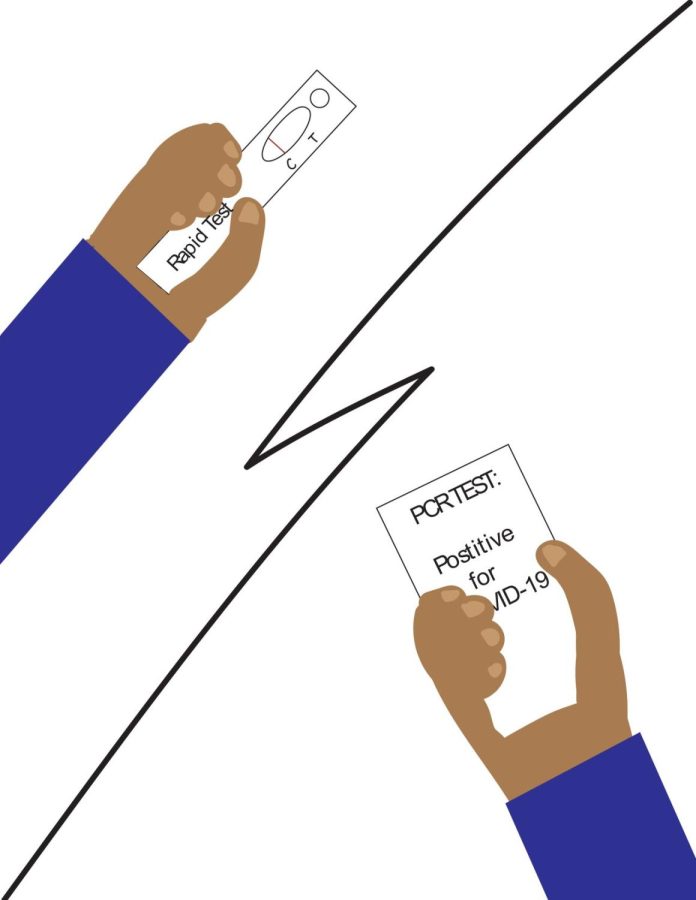
An instant test, an instant negative
The contradicting results from an antigen test and a PCR test cause many issues, regarding false positives and false negatives.
“Please note that negative results do not rule out COVID-19,” according to the instructions of the iHealth RapidTest. This statement is something that people seem to disregard or put to the side despite the user’s result. The iHealth RapidTest is the most commonly used brand for COVID-19 rapid testing as they were being distributed to the public for free.
During the surge of the COVID-19 virus and its variants during winter, lines for COVID-19 have increased. On Monday Jan. 10, San Diego County testing site averaged four hours and San Marcos Test Site at California State University San Marcos said to have been administering 1,500 tests daily. COVID-19 rapid tests have become more prevalent due to the easier and convenient results. These tests allow people to test for COVID-19 within any place at any time.
Rapid tests, also called an antigen test, are made to detect proteins in the virus which causes COVID-19. However, a molecular test or more specifically a Polymerase Chain Reaction (PCR) test, detects genetic material that is specific to the virus that causes COVID-19.
In a study conducted by JAMA Network, the validity of antigen tests to PCR tests were compared to each other. From 0-12 days of people with COVID-19 symptoms, 78.9 percent of people were correctly identified with the virus while 97.1 percent of people were correctly identified without the virus.
The antigen tests’ accuracy depends on how much of the virus was in the sample at that specific time the test was taken. The longer an individual was infected with COVID-19, the more of the virus expands through the body, allowing the test to better detect the virus. In contrast, PCR tests are generally highly sensitive and specific as they look for more genetic material, specifically Ribonucleic acid (RNA), making them more accurate.
According to a study done by respiratory medicine professors at the University of Thessaly Dimitra Mouliou and Konstantinos Gourgoulianis, false antigen test results arise when test procedures are incorrectly followed or used by untutored users.
Human error could also be a contributor to the low reliability of a rapid test. People simply not following the directions may disrupt the accuracy. The nasal swab might not detect proteins because it was not fully swirled around the nose or the COVID-19 proteins did not diffuse into the tube of liquid.
A false negative would cause a person to believe that they are negative, persuading the person to go on with their daily lives despite them having COVID-19. This would result in the virus spreading to other people. On the other hand, a false positive would cause a person to believe that they’re negative, causing them to cancel scheduled events and stay home, overall making them unproductive.
On a fact sheet written by the Center for Disease Control (CDC) 2019-nCoV Real-Time RT-PCR Diagnostic Panel, “risks to a patient of a false negative test result include: delayed or lack of supportive treatment, lack of monitoring of infected individuals and their household or other close contacts for symptoms resulting in increased risk of spread of COVID-19 within the community, or other unintended adverse events.”
The best test available to the public for the most accurate result would be a PCR test. Bonita Vista High administered free iHealth rapid tests before resuming school after Winter Break which may have missed COVID-19 in students allowing the transmission of the virus to other students. It is important for people suspected of having COVID-19 to get tested and self-isolate in order to treat themselves. Overall, staying healthy is very crucial for the development and the course of life.

I am a junior at Bonita Vista High and this is my first year on staff for the Crusader. I joined the newspaper because of an interest that was inspired...

As a senior and Editor-in-Chief of BVH’s the Crusader, I hope to guide the publication to continue publishing articles that have an impact on our community....